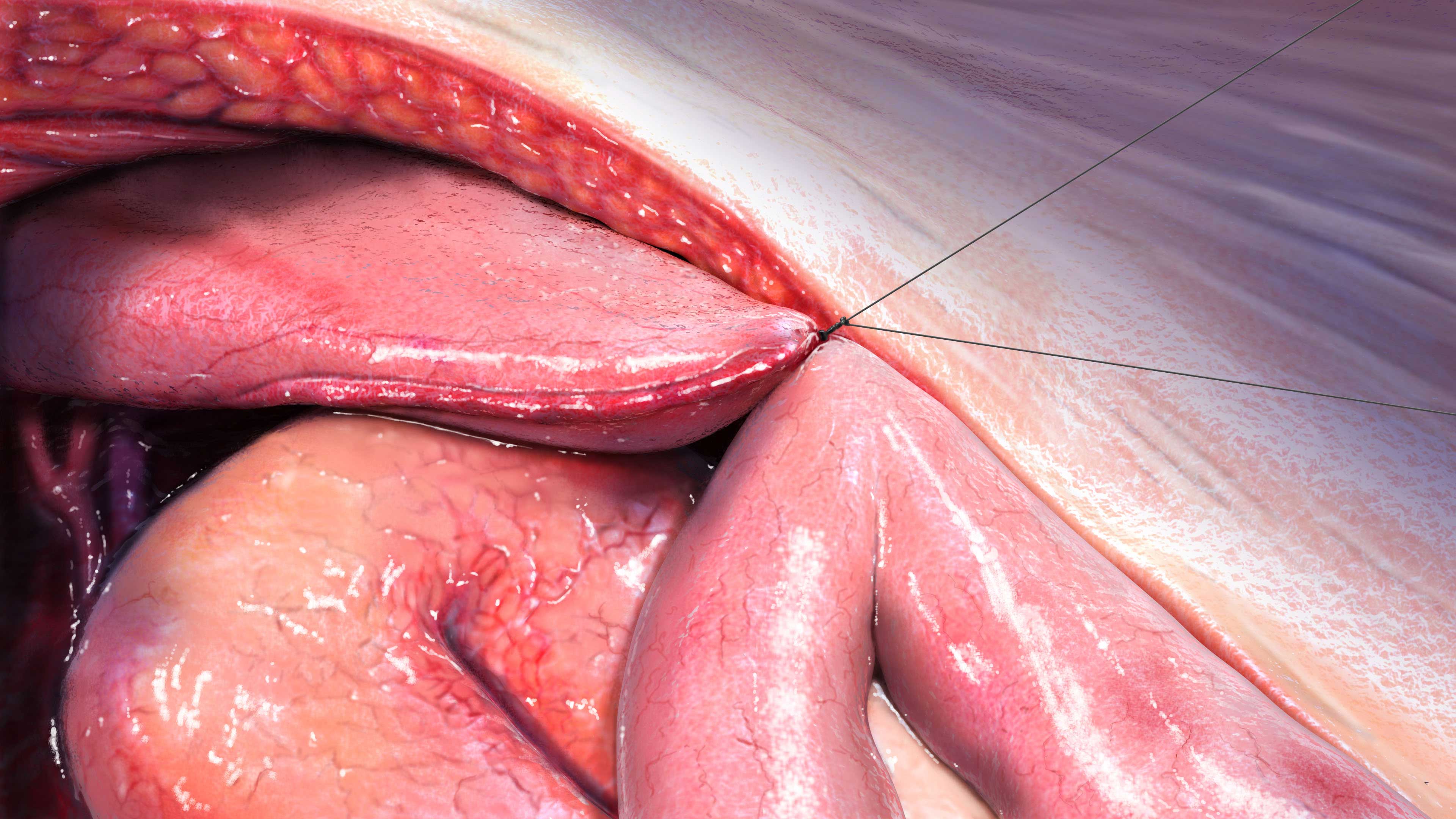
Gastrointestinal (Including Pancreatic) Surgery
About
Patients may undergo gastrointestinal (GI) surgery for many reasons, including chronic pancreatitis, cancer, Crohn’s disease and trauma. Depending on the anatomical area of surgery and the specific procedure used, pancreatic exocrine insufficiency (PEI) may result, as either a direct or indirect consequence.1-3
Epidemiology
PEI has been found to occur in more than 80% of patients after GI surgery, including pancreatic surgery.4
Patients may develop PEI after partial or total gastrectomy and duodenopancreatectomy.4 In patients with pancreatic cancer, PEI is seen in 80% of patients after surgery.2 Central pancreatic resection is associated with a lower rate of PEI, and distal pancreatectomy may preserve pancreatic exocrine function altogether.3
Causes
Major pancreatic resection decreases pancreatic secretory capacity, including exocrine secretion, and the pathology and the type and extent of resection are factors which determine whether a patient will develop clinical signs of PEI.1-3
Patients may develop PEI to some extent after gastric surgery, but in patients with more severe bowel symptoms, PEI can contribute to maldigestion and weight loss, which affects their quality of life.3 Partial or total gastrectomy may be associated with reduced pancreatic enzyme secretion after a meal, mainly because of asynchrony between gastric emptying, release of bile and pancreatic enzymes into the small intestine (postcibal asynchrony), but also denervation of the pancreas following vagotomy.1,3 Pancreatico-biliary bypass results in extreme asynchrony.3
Reduced endogenous stimulation and postcibal asynchrony may also result following extensive small bowel resections.1,3 GI adaptation following extensive small bowel resectioning lead to compensatory increases in the secretion of gastrin and pentagastrin into the plasma, which are thought to affect the size and composition of the pancreas.3 Furthermore, bacterial overgrowth may cause premature enzyme degradation.3
Pathophysiology
Pancreatic cancer and chronic pancreatitis are indications for pancreatic surgery.2 For further information on the pathophysiologies of pancreatic cancer and chronic pancreatitis, CLICK BELOW.
Gastric surgery is sometimes indicated for the treatment of gastric cancer, severe peptic ulcers uncontrolled by medication, or its complications.3 Pancreatico-biliary bypass, which also removes part of the stomach, is a procedure used to treat severe obesity.3
Small bowel resections are used to treat Crohn’s disease, tumours, ischaemia, and trauma. Pancreatico-biliary bypass also functionally removes a large part of the small bowel.3
FACT
Most patients experiencing PEI following pancreatic surgery are undertreated. More focus is needed on treating PEI and educating patients to adjust their PERT doses according to their symptoms and diet.
Sikkens et al., 20122
Signs and Symptoms
In general, PEI causes malabsorption and maldigestion, resulting in symptoms of:2,3
Symptoms
- WEIGHT LOSS
- ABDOMINAL PAIN
- FATIGUE
- DIARRHOEA
- STEATORRHOEA
- FLATULENCE
Steatorrhoea, characterised by foul-smelling, greasy stools, is a typical clinical manifestation of severe PEI.3,4 Malabsorption associated with PEI, characterised by steatorrhoea, weight loss and malnutrition, is associated with deficiencies of fat-soluble vitamins: A, D, E and K, minerals, and essential fatty and amino acids.2,4
In patients with pre-existing chronic pancreatitis, the percentage of patients with steatorrhoea can increased markedly after resection.1
Complications
Complications from maldigestion and malabsorption may have a progressive and detrimental effect on a patient’s wellbeing, impact the outcome of the underlying disease, and increase morbidity and mortality.2,4 For further information on the complications of PEI, CLICK HERE.
Diagnosis of PEI
There are several methods available for diagnosing PEI, with the indirect methods being the most frequently used in the clinical setting. Of these, the 3-5 day faecal fat balance test is recommended because it has been shown to correlate well with direct tests of pancreatic function.3
For more information on diagnosing PEI, CLICK HERE.
Treatment
Generally, post-surgical PEI may be managed similarly to PEI resulting from chronic pancreatitis.4
To learn more about the treatment of PEI associated with chronic pancreatitis, CLICK HERE.
Pancreatic surgery: The severity of PEI may vary, and therefore the dosage of PERT should be individualised. Typically, 25,000-50,000 units of lipase is required with every meal. Adjunctive therapy with acid suppressants may be required.3
Gastric surgery: The symptoms of PEI which may follow gastric surgery can be improved, although not completely reversed, by PERT. It should be considered in cases of severe steatorrhoea. PERT doses should be individualised. In general, 25,000-40,000 units of lipase should be given with each regular meal, and 10,000 units with each small meal or snack.3
Small bowel resection: In cases where there are symptoms of PEI, PERT is recommended as a component of treatment following major resection of the small bowel. Standard lipase doses (25,000-40,000 IU) for regular meals, and 10,000 IU for smaller meals or snacks should be prescribed. In extreme cases, total parenteral nutrition may be necessary initially. Adjunctive pharmaceutical treatments may include antimotility agents to slow intestinal transit, compensatory bile-acid resins, gastric acid hypersecretion suppressants, antibiotics and/or probiotics to suppress intestinal bacterial overgrowth, and/or recombinant human growth hormone to enhance intestinal adaptation and hence improve nutrient absorption.3
To learn more about the treatment of PEI with PERT, dosing of PERT, and other aspects of PEI management, CLICK HERE.
Long-term management and monitoring for PEI in patients with GI surgery
Following pancreatic surgery, all patients should be screened and monitored for indications of inadequate enzyme replacement, including weight loss, diarrhoea, steatorrhoea, and stool fat excretion of >15 g/day.3
In cases of bowel resection, adjustment of nutrition is complex and should be personalised. Referral to a dietician is recommended.3
References
- Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54(Suppl VI):vi1–vi28.
- Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. The daily practice of pancreatic enzyme replacement therapy after pancreatic surgery: a Northern European survey. enzyme replacement after surgery. J Gastrointest Surg. 2012;16:1487–1492.
- Smith RC, Smith SF, Wilson J, Pearce C, Wray N, Vo R, et al. Australasian guidelines for the management of pancreatic exocrine insufficiency. Australasian Pancreatic Club. October 2015. pp 1–122.
- Domínguez-Muñoz JE. Pancreatic exocrine insufficiency: diagnosis and treatment. J Gastroenterol Hepatol. 2011;26(Suppl 2):12–16.
PEI and Gastrointestinal (Including Pancreatic) Surgery Quiz


