PEI and Chronic Pancreatitis
About
Chronic pancreatitis is the most common cause of PEI.1 Chronic pancreatitis has several causes and the inflammation results in the persistent loss of pancreatic tissue and impaired function.2 Both endocrine and exocrine tissues are irreversibly damaged.2 In patients with chronic pancreatitis, destruction of the pancreatic tissue results in PEI due to the loss of the ability to produce pancreatic enzymes.1
Epidemiology
The reported incidence of chronic pancreatitis in industrialised countries ranges from 3.5 to 10 per 100,000 people2 and increases with age.3 The prevalence is estimated to be from 28.5 to 41.8 per 100,000 people, and is most common in adult males.3 The prevalence of PEI within this patient population varies with severity of chronic pancreatitis, from an estimated 30% in mild cases to 85% in severe cases.3
Causes
Chronic pancreatitis may be caused by environmental, autoimmune, and genetic factors2,3
- Alcohol
- Autoimmune
- Idiopathic
- Trauma
- Inherited factors
- Congenital
- Hyperparathyroidism
- Hyperlipidaemic
- Due to cystic fibrosis
- Due to protein-energy malnutrition
Of these, environmental factors are the most common, with excessive alcohol intake accounting for 70-80% of cases.3 Smoking is also a dose-dependent contributing factor to chronic pancreatitis development and progression, especially when combined with alcohol abuse.3
In adults, approximately 10% of chronic pancreatitis cases are idiopathic.3
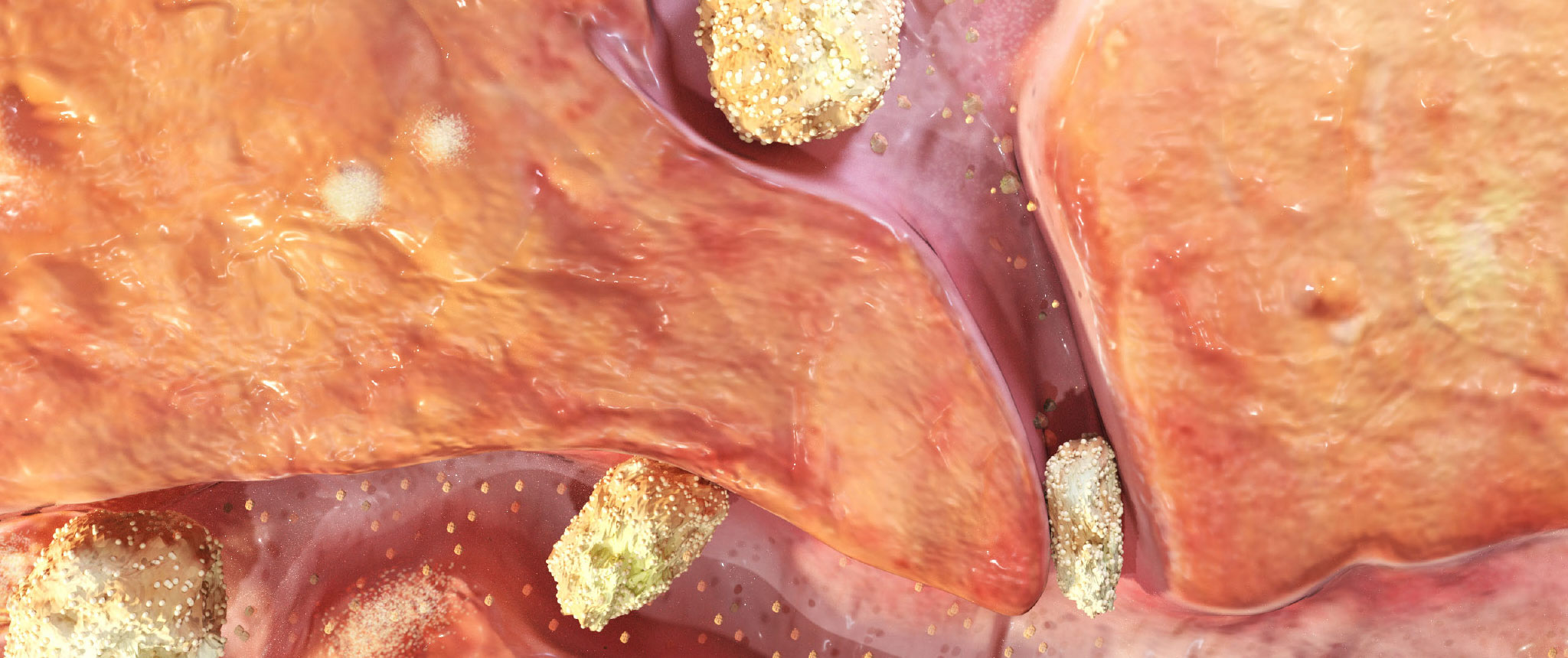
Pathophysiology
The inflammation in chronic pancreatitis has several pathophysiological characteristics including:4
- Fibrosis of pancreatic tissue
- Pancreatic duct dilation
- Calcifications in the pancreatic ducts or parenchyma
- Endocrine and exocrine dysfunction
In addition, acute inflammation, fat necrosis, and pancreatic pseudocysts may be present.2
The destruction of pancreatic ductal and acinar cells reduces the ability of the pancreas to produce the digestive enzymes amylase, lipase, and protease. This results in maldigestion and malabsorption.3,5
When excessive alcohol is the cause of chronic pancreatitis, symptoms of PEI usually occur after 10-15 years of abuse.3
PEI has been found to be a significant independent risk factor for increased mortality in patients with chronic pancreatitis.6
Despite loss of pancreatic function in PEI, the digestion of carbohydrates and proteins can be reasonably well compensated for by other parts of the digestive tract. Fat digestion, however, is more complicated and pancreatic lipase is an essential part of the process which cannot be compensated for by other enzymes.2
Fat absorption is particularly affected in PEI3:
- The pancreas is the main source of lipase production for the digestion of fat
- The ability of the pancreas to produce and secrete lipase is impaired earlier and to a greater extent than other pancreatic enzymes, especially in chronic pancreatitis
- Lipase activity in the stomach cannot compensate for the loss of pancreatic lipase production
- In PEI the pancreas fails to secrete the normal amount of sodium bicarbonate which protects pancreatic enzymes from denaturation by gastric acid
- The low pH deactivates bile acids, reducing the solubilization of fat
- Chronic pancreatitis patients with PEI need pancreatic enzyme replacement therapy (PERT) to improve nutrient digestion and absorption4
FACT
In healthy individuals, stomach lipase activity accounts for about 10% of fat digestion, but this rises to more than 90% in patients with PEI.
Suleiman SL, et al. 20123
Signs and symptoms
The three main clinical features of chronic pancreatitis and associated PEI are abdominal pain, maldigestion and diabetes.2
Maldigestion, caused by PEI, occurs relatively late in chronic pancreatitis because it only becomes evident when production of digestive enzymes falls below 10% of normal secretion.
PEI causes malabsorption and maldigestion, resulting in symptoms of:2,7
Symptoms
- WEIGHT LOSS
- ABDOMINAL PAIN
- FATIGUE
- DIARRHOEA
- STEATORRHOEA
- FLATULENCE
Steatorrhoea, which is characterized by foul-smelling, greasy stools, is the most classical clinical manifestation of PEI, but may not appear until the disease is advanced.2,8
Steatorrhoea occurs in about 30% of patients with chronic pancreatitis and may be associated with deficiencies of fat soluble vitamins: A, D, E and K, leading to osteoporosis and other complications.2
Diabetes can be a late-stage symptom of chronic pancreatitis because as well as damage to the exocrine pancreas, endocrine function is also affected. This is categorized as Type IIIc diabetes, and includes destruction of insulin-secreting cells and glucagon-secreting cells.2
Complications
Complications from maldigestion and malabsorption may have a progressive and detrimental effect on a patient’s wellbeing and may impact the outcome of the underlying disease, and increase morbidity and mortality.9,10 For a full discussion on complications of PEI, CLICK HERE.
Diagnosis
PEI is a late-stage development in patients with chronic pancreatitis, and may be easily diagnosed with specific methods, along with imaging techniques to aid the diagnosis of advanced pancreatitis. It is early pancreatitis that presents a diagnostic challenge.2
Chronic pancreatitis patients with abdominal pain, diarrhoea, nutritional deficiencies, and unintentional weight loss should be tested for PEI.2
There are several methods available for diagnosing PEI, with the indirect methods being the most frequently used in the clinical setting. For a detailed discussion of these techniques, CLICK HERE.
Treatment
Pancreatic enzyme replacement therapy (PERT) is the standard treatment for PEI.2
In patients with chronic pancreatitis and associated PEI, PERT has demonstrated benefits in fat absorption, stool frequency and fat content, flatulence, abdominal pain, body weight, BMI, and improvements in quality of life.11
Study design11
A 51-week, open-label extension of a 1 week multicentre, double-blind, randomized, placebo-controlled trial conducted in India enrolled 61 adult patients with chronic pancreatitis and confirmed PEI. Patients received pancreatin (pancrelipase) at a dose of 80,000 Ph. Eur. Lipase units with each of three main meals per day, plus an additional 40,000 units with each snack (up to three per day).
After 51 weeks of pancreatin treatment, patients with PEI due to chronic pancreatitis showed significant improvements compared with baseline in a. stool frequency, b. body weight and c. BMI.



To learn more about the treatment of PEI with PERT, dosing of PERT, and other aspects of PEI management, CLICK HERE.
References
- Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54(Suppl 6):vi1-28.
- Smith RC, Smith SF, Wilson J, Pearce C, Wray N, Vo R, et al. Australasian guidelines for the management of pancreatic exocrine insufficiency. Australasian Pancreatic Club, October 2015. pp 1-122.
- Suleiman SL, Kadiyala V, Conwell DL. Pancreatic exocrine insufficiency. Part 1 of 2: Pathogenic and Diagnostic Considerations. Gastroenterology and Endoscopy News, Special Edition, 2012. pp51-56. Available from: http://www.gastroendonews.com/download/Pancre_CaPart1GENSE12_WM.pdf. Last accessed: November 2017.
- Thorat V, Reddy N, Bhatia S, Bapaye A, Rajkumar JS, Kini DD, et al. Randomised clinical trial: the efficacy and safety of pancreatin enteric-coated minimicrospheres (Creon 40000 MMS) in patients with pancreatic exocrine insufficiency due to chronic pancreatitis: a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2012;36(5):426-36.
- Imrie CW, Connett G, Hall RI, et al. Review article: enzyme supplementation in cystic fibrosis, chronic pancreatitis, pancreatic and periampullary cancer. Aliment Pharmacol Ther. 2010;32(Suppl 1):1-25.
- de la Iglesia-Garcia D, Vallejo-Senra N, Iglesias-Garcia J, López-López A, Nieto L, Domínguez-Muñoz JE. Increased Risk of Mortality Associated With Pancreatic Exocrine Insufficiency in Patients With Chronic Pancreatitis. J Clin Gastroenterol. 2017 Aug 30. doi: 10.1097/MCG.0000000000000917.
- Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. Patients with exocrine insufficiency due to chronic pancreatitis are undertreated: a Dutch national survey. Pancreatology. 2012;12(1):71-73.
- Leeds JS, Oppong K, Sanders DS. The role of fecal elastase-1 in detecting exocrine pancreatic disease. Nat Rev Gastroenterol Hepatol. 2011;8:405-15.
- Ockenga J. Importance of nutritional management in diseases with exocrine pancreatic insufficiency. HPB (Oxford). 2009;11(Suppl 3):11-15.
- Fitzsimmons D, Kahl S, Butturini G, van Wyk M, Bornman P, Bassi C, Malfertheiner P, George SL, Johnson CD. Symptoms and quality of life in chronic pancreatitis assessed by structured interview and the EORTC QLQ-C30 and QLQ-PAN26. Am J Gastroenterol. 2005;100(4):918-926.
- Ramesh H, Reddy N, Bhatia S, et al. A 51-week, open-label clinical trial in India to assess the efficacy and safety of pancreatin 40000 enteric-coated minimicrospheres in patients with pancreatic exocrine insufficiency due to chronic pancreatitis. Pancreatology. 2013;13(2):133-9.


