Inflammatory Bowel Disease
About
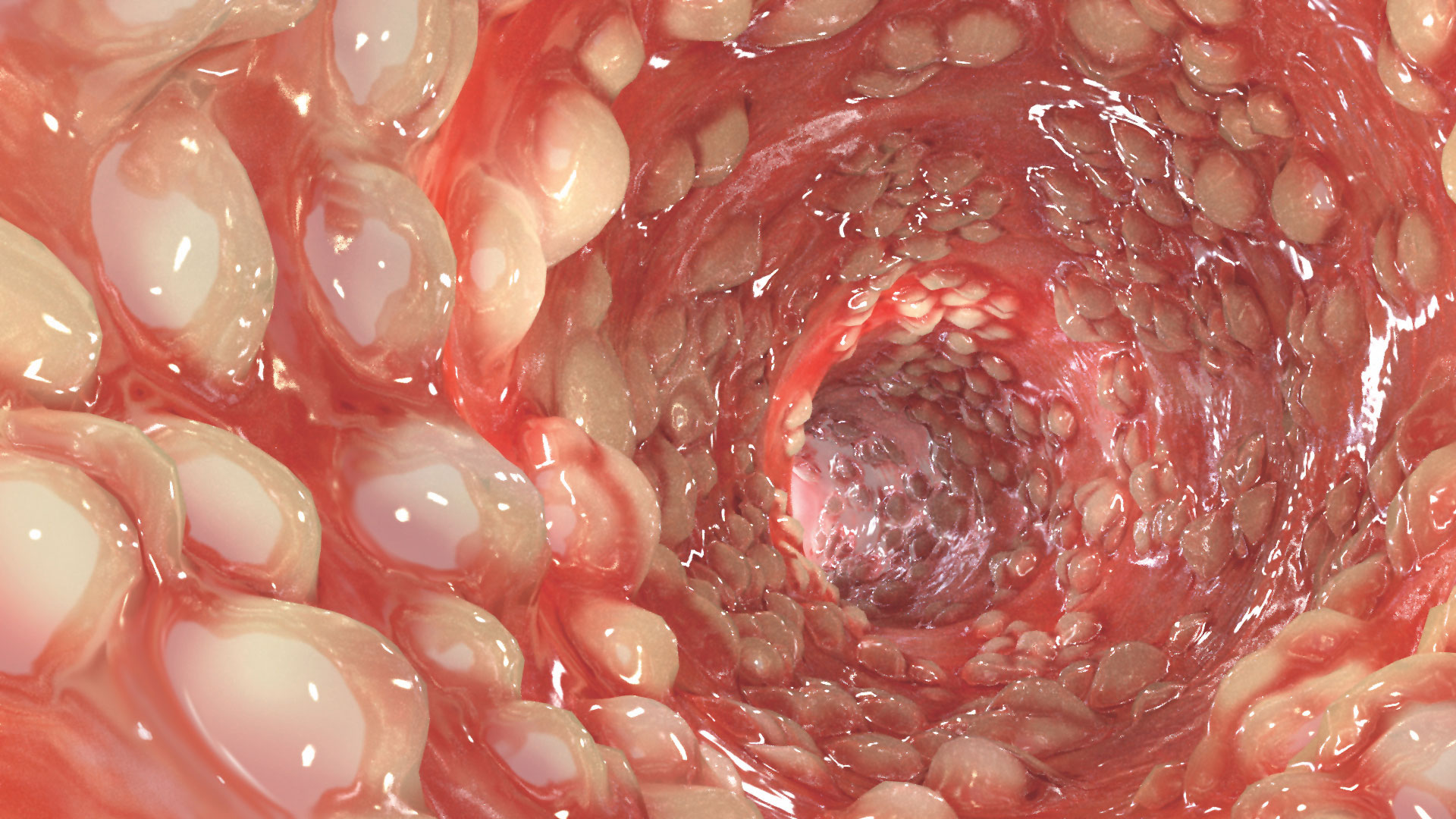
Inflammatory bowel disease (IBD) is a term that includes Crohn’s disease and ulcerative colitis. Genetic factors, environmental influences and the intestinal microflora combine to produce an abnormal immune response and the characteristic inflammation in the bowel. IBD may affect several organs other than the intestines. Pancreatic abnormalities in IBD are common and include acute and chronic pancreatitis, autoimmune pancreatitis, and asymptomatic pancreatic abnormalities.1,2 Patients with IBD are at risk for developing PEI, particularly if they have at least three bowel movements per day, loose stools, and a history of surgery.3
Epidemiology
Pancreatic exocrine insufficiency (PEI) has been found in 21% of patients with IBD using the para-aminobenzoic acid (PABA) test. In Crohn’s disease specifically, PEI based on low faecal elastase-1 levels has been seen in 14-30% of patients, and abnormal fat excretion seen in 17-35% of patients. In ulcerative colitis, 22% of patients have PEI based on faecal elastase-1 levels ≤200 μg/g, and 50% have bicarbonate and/or enzyme insufficiency.3
Causes
It is unclear why pancreatic secretion is reduced in IBD. In Crohn’s disease, it may be caused by malnutrition, or by inflammation and/or scarring in the intestinal wall. Direct damage to the pancreas may also be a factor.2
PEI has also been described in patients with IBD without clinical symptoms. This PEI is thought to be transient, at least in some patients.1
PEI may be also associated with chronic pancreatitis in patients with IBD.1,2 In most of these cases, chronic pancreatitis is idiopathic.1 It has been suggested that chronic pancreatitis is, in fact, an extraintestinal manifestation of IBD.1
For more information on the causes of PEI in chronic pancreatitis, CLICK HERE.
Pathophysiology
The pathophysiology of PEI in IBD is unclear. Possible mechanisms in Crohn’s disease include pancreatic autoantibodies (present in about one third of patients), duodenal reflux, and reduced secretory hormone production.2,3 Scarring or inflammation may reduce intestinal hormone secretion, which can reduce pancreatic exocrine function due to insufficient stimulation. In both Crohn’s disease and ulcerative colitis, pathological changes have been seen in the pancreatic duct which may impede the flow of digestive enzymes.3
FACT
Patients with IBD who are showing symptoms of PEI may benefit from pancreatic enzyme replacement therapy (PERT).
Keller and Layer, 20054
Signs and Symptoms
In most cases, PEI in IBD patients are considered mild to moderate in severity. However, patients with Crohn’s disease who have reduced absorptive capacity due to extensive inflammation, small intestinal resections or scars, or motility disturbances, may become symptomatic.4
In general, PEI causes malabsorption and maldigestion, resulting in symptoms of:5,6
Symptoms
- WEIGHT LOSS
- ABDOMINAL PAIN
- FATIGUE
- DIARRHOEA
- STEATORRHOEA
- FLATULENCE
Steatorrhoea, which is characterised by foul-smelling, greasy stools, the most common clinical manifestation of EPI, may not appear until the disease is severe6,7, or in the case of patients with Crohn’s disease, less severe PEI may become symptomatic due to reduced absorptive capacity.4
Complications
Complications from maldigestion and malabsorption may have a progressive and detrimental effect on a patient’s wellbeing, and may impact the outcome of the underlying disease and increase morbidity and mortality.8-10 For further information on the complications of PEI, CLICK HERE.
Diagnosis of PEI
There are several methods available for diagnosing PEI, with the indirect methods being the most frequently used in the clinical setting.6 Of these, faecal elastase screening for pancreatic function is the preferred test, with the faecal fat test and the breath test being alternative options.11
For more information on diagnosing PEI, CLICK HERE.
Treatment
Although there is a relatively high prevalence of PEI in patients with IBD, there is no clinical data or guidelines on the use of pancreatic enzyme replacement therapy (PERT) in these populations and on how effective it might be.3
To learn more about the treatment of PEI associated with chronic pancreatitis CLICK HERE.
To learn more about the treatment of PEI with PERT in general, dosing of PERT, and other aspects of PEI management, CLICK HERE.
References
- Roque Ramos L, Sachar DB, DiMaio CJ, Colombel JF, Torres J. Inflammatory bowel disease and pancreatitis: a review. J Crohns Colitis. 2016;10(1):95-104.
- Antonini F, Pezzilli R, Angelelli L, Macarri G. Pancreatic disorders in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2016;7(3):276–282.
- Singh VK, Haupt ME, Geller DE, Hall JA, Quintana Diez PM. Less common etiologies of exocrine pancreatic insufficiency. World J Gastroenterol. 2017;23(39):7059–7076.
- Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54(Suppl VI):vi1–vi28.
- Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. The daily practice of pancreatic enzyme replacement therapy after pancreatic surgery: a Northern European survey. enzyme replacement after surgery. J Gastrointest Surg. 2012;16:1487–1492.
- Smith RC, Smith SF, Wilson J, Pearce C, Wray N, Vo R, et al. Australasian guidelines for the management of pancreatic exocrine insufficiency. Australasian Pancreatic Club. October 2015. pp 1–122.
- Domínguez-Muñoz JE. Pancreatic exocrine insufficiency: diagnosis and treatment. J Gastroenterol Hepatol. 2011;26(Suppl 2):12–16.
- Sikkens EC, Cahen DL, van Eijck C, Kuipers EJ, Bruno MJ. Patients with exocrine insufficiency due to chronic pancreatitis are undertreated: a Dutch national survey. Pancreatology. 2012;12(1):71-73.
- Ockenga J. Importance of nutritional management in diseases with exocrine pancreatic insufficiency. HPB (Oxford). 2009;11(Suppl 3):11-15.
- Fitzsimmons D, Kahl S, Butturini G, van Wyk M, Bornman P, Bassi C, Malfertheiner P, George SL, Johnson CD. Symptoms and quality of life in chronic pancreatitis assessed by structured interview and the EORTC QLQ-C30 and QLQ-PAN26. Am J Gastroenterol. 2005;100(4):918-926.
- Thomas PD, Forbes A, Green J, et al. Guidelines for the investigation of chronic diarrhoea, 2nd edition. Gut. 2003;52(Suppl 5):v1–15.


